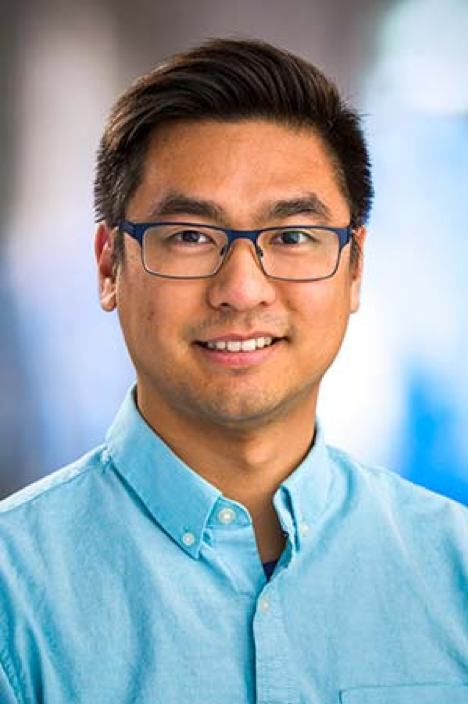
Today’s installment is with BBI member Dr. Gavin Ha, Assistant Professor, Computational Biology Program in the Public Health Sciences and Human Biology Divisions at Fred Hutchinson Cancer Research Center
BBI: Thanks for speaking with us today!
Gavin Ha: Thanks, I’m happy to!
BBI: Kicking things off, how do you view your work in cell-free DNA as relating to precision medicine?
Gavin Ha: We apply novel computational probabilistic approaches to help us tease out trace amounts of cell-free DNA signal in large amounts of genetic data that would otherwise be difficult to isolate. In general, there is a benefit to knowing tumor DNA exists in a sample, but there is great use in developing sensitive algorithmic tools to answer the question, “How much is there?” We have been able to use this quantitative data to correlate with how a tumor progresses, and to understand if a patient is responding to treatment or not.
Another area where a computational approach can help address a problem is coming up with ways that nucleosome footprints can tell us about other “omics” data from cell free DNA. this allows us to move beyond the genotype of a sample, and instead look at the phenotype of that sample. When we start looking at gene expression and transcriptional regulation, these are all processes that allow us to infer how that genotype is being expressed in a given patient sample. Beyond looking at genetic information we get from cell-free DNA, we can begin to look at gene expression, transcriptional regulation, and the epigenome as well. Typically, teasing out these different pieces of information requires multiple assays from tumor tissue, but we can now integrate these analyses from a single standard cell free DNA assay using only computational methods.
BBI: Can you give us an example of how these computational approaches are being put to use?
Gavin Ha: Sure, prostate cancer is a major research interest for our group and collaborators. One of the potential resistance mechanisms often found in prostate cancer happens when patient tumor cell types can transdifferentiate into another cell type during treatment resistance. For example, prostate cancer that often starts as an adenocarcinoma can differentiate itself into an especially difficult to treat neuroendocrine cancer. This is often a much more aggressive cancer, with many fewer available therapies. The field has done a lot of work to understand how to sensitively detect circulating cell-free tumor DNA from prostate adenocarcinoma. We are exploring whether we can detect, and be able to sensitively predict, a change in a patient’s cancer phenotype all from a single blood-draw. That of course could inform prognosis and treatment, but also could reveal potential biomarkers for understanding cell plasticity in prostate cancer.
We have a few other collaborations with folks at Fred Hutch/UW and at other institutions to study circulating tumor DNA in lung, breast, and pediatric cancers.
BBI: How has your work been supported by BBI?
Gavin Ha: The BBI Catalytic Collaborations grant allowed us to establish a new collaboration with UW Medicine and Colin Pritchard’s group. We were able to look at low-pass whole genome sequencing cell-free DNA through the group’s clinical sequencing platforms. Because we were able to work with an established clinical sequencing platform, the quality of the data we got was excellent. From the standpoint of data analysis, any of the computational methods we create will have the opportunity to be translated into the clinic and hopefully make an impact for patient diagnostics.
BBI: Where do you see this work headed in the next 10-20 years?
Gavin Ha: My hope is that cfDNA will move in the direction of powerful real-time monitoring of disease. For patients with cancer, I hope we can move to a place where we are regularly assessing where a patient’s cancer is heading at a genetic and molecular level with routine blood tests. It would be incredible if we could get to a place where we have sensitive algorithms and validated assays that allow us to monitor cancer progression in real-time. As with prostate cancer that we talked about earlier, this could potentially help to detect changes in a patient’s cancer state well before it is otherwise clinically detectable.
For patients without cancer, or patients in remission, the ultimate hope of cfDNA would be to use blood draws to detect molecular changes that help to predict or diagnose asymptomatic cancer before it would otherwise be clinically detectable.
BBI: Thanks for telling us more about your work Dr. Ha.
Gavin Ha: Of course, and thank you!