BBI: How do you view your work as relating to precision medicine?
Tim Cherry: My background is in the basic development of the nervous system, and in the retina in particular. The driving problem in our work is to expand the search space for disease-causing mutations in the visual system. In recent years, we’ve worked to understand what genes are required for normal retinal function, and how the non-coding genome is involved as well. A lot of work done around the world, including some really important work done here at UW, has demonstrated that the non-coding genome plays an important role in the development of human disease. We aim to shine light on the less understood areas of the genome to understand what functional elements of the non-coding genome might be compromised in retinal disease.
BBI: How have you approached this work recently?
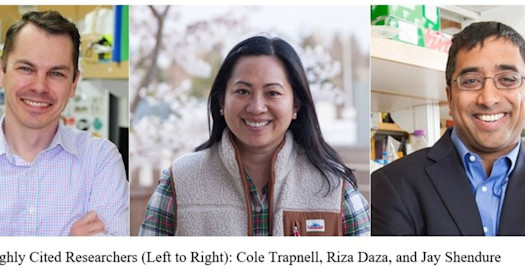
Tim Cherry: We have focused this work in two main ways. The first is a descriptive approach. We have helped define the epigenetic signatures of functional elements of the non-coding genome related to visual function using tools like DNAase-seq, ATAC-seq, and through mapping transcription factor binding and histone modifications. Thanks to the work of other BBI members like Cole Trapnell, Jay Shendure, Steve Henikoff, and others, we are now able to do this work at the single-cell level.
Secondly, thanks to BBI we’ve been able to start a collaboration with a fantastic group of machine-learning experts. We are training machine learning models using this epigenomic data that we’ve spent the last five years collecting, teaching the machines the features of DNA sequences that are required to have a functional DNA enhancer or promoter that drives essential gene expression. These models are learning how to recognize when a mutation in one of these non-coding regions is likely to be disease-causing or not.
To give you an example, we have been following a single nucleotide change in an enhancer that is about 150 kb away from the nearest gene. That variant seems to be sufficient to cause a relatively early onset inherited visual disorder. This is a pretty extreme example of a non-coding mutation driving disease, but there are more subtle examples too. We are beginning to develop tools to understand non-coding mutations that might not normally be pathogenic, but can modify disease in some individuals who are predisposed by non-genetic factors. In these circumstances, one member of a family can have severe retinal disease, while another member can have relatively mild disease.
Understanding these sorts of drivers and modifiers of disease is one of the principal goals of precision medicine as I see it.
Tim Cherry: ‘This is a poster child for precision medicine’s promise”
BBI: Can you tell us more about how the machine learning group got started and what you are working on?
Tim Cherry: Absolutely. I met BBI member and ophthalmologist Dr. Aaron Lee at a conference in New York. We had been intrigued by each other’s work for a while, and he had a strong background in the use of machine learning programs that had shown the ability to diagnose retinal disease. After continuing to talk, it became clear the BBI catalytic collaborations grant was the perfect vehicle for us to collaborate.
We worked to find individuals with unexplained visual disorders that looked to be mendelian in nature. A lot of visual disorders tend to be recessive disorders, and one reasonably common one is called Stargardt Disease. It is almost always caused by mutations in a particular gene called ABCA4, which is necessary for recycling the components of the visual cycle. Working together, we had identified individuals who had one identified coding mutation, but mysteriously seemed to lack the second mutation normally required for this recessive disease to manifest.
It was our hypothesis that the second mutation would be in the regulatory element of the non-coding genome. The problem with these sorts of non-coding mutations is that they are numerous and very hard to link back as a contributor to the disease. There are too many variants than are practical to screen. We developed a pipeline for initially vetting modifier alleles in associated promoters and enhancers using machine learning to help us prioritize which mutations we should follow up with. Within the BBI community, we have gotten help from many others including BBI member Mike Bamshad and his Center for Mendelian Genomics at UW.
We were sitting on a mountain of data that we were able to make useful through the powerful computational techniques that Aaron’s group had been developing. We are putting together our first manuscript on this right now, and the results are very exciting. I hold this up as a real success story of BBI pilot grants because it has blown open the gates with leads for future research. BBI allowed us to have the bandwidth and funding to hammer out a collaboration between our research team and our clinical colleagues.
BBI: Knowing that research can take a long time to come to fruition, what is your hope for the promise of precision medicine in your field?
Tim Cherry: In the next five to ten years, given the convergence of technologies that are available, I have a lot of optimism for the improvement of genetic diagnostics. Once we become better at precisely diagnosing genetic disorders, we have paved the path to the door of therapeutic innovation. For the first time ever, there has recently been a gene replacement therapy made available for a retinal disorder. Though it is at this point only a possibility for a very small slice of people with a very specific retinal disorder, this is a poster child for precision medicine’s promise.